Abstract
Background Augmenting adaptive immunity through immune checkpoint blockade introduced a paradigm shift in the treatment of cancer patients. Although aberrant mRNA upregulation of several immune checkpoints (e.g. PDL1) has been described in CD34+ cells of myelodysplastic syndrome (MDS) patients compared to normal controls (Yang et al ., 2014), clinical investigations of checkpoint inhibitors in myeloid malignancies to-date have shown low response rates to monotherapy with a lack of response biomarkers. MDS is genetically heterogeneous evidenced by the array of somatic gene mutations that may impact differential checkpoint display. In concordance, our interrogation of the AML TCGA dataset identified TP53 mutant (MT) AML as an immunologically distinct subset with checkpoint upregulation. Therefore, our goal was to comprehensively characterize checkpoint molecules by lineage and stage of maturation in MDS to discern relationships with immune cell subsets in molecularly defined cohorts.
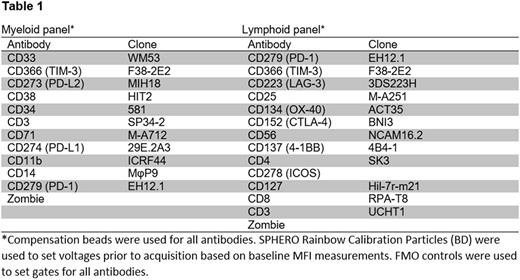
Patients and Methods Utilizing the Moffitt Cancer Center tissue core and MDS database, bone marrow mononuclear cells were obtained from genetically profiled MDS (n=23), CMML (n=5) and secondary AML patients (n=22). NGS of up to 54 genes was performed at the time of sample acquisition with 5% VAF threshold and 500x minimum depth of coverage. Multi-color flow cytometry acquisition of immune checkpoints with a myeloid and lymphoid panel (Table 1) was performed using a BD LSRII, and analysis was conducted using FlowJo v10.3. Clinical variables and outcomes of patients were characterized at the time of sample procurement. Mann-Whitney and Kruskal-Wallis tests were used for comparative analyses. Median values of each checkpoint were calculated to compare outcomes of patients with increased versus decreased expression. Kaplan-Meier curves were used to estimate OS and analyzed from the date of sample collection. Multivariate Cox regression models were created to adjust for clinical characteristics.
Results A total of 50 patients were analyzed (25 TP53 MT and wildtype (WT), respectively) with a median age of 72 years and male predominance (58%). Overall 38% of patients (n=19) were treatment naïve while 40% were HMA refractory (n=20). TP53 MT patients had significantly higher percentage of PDL1+ hematopoietic stem cells (HSC; Lin-/CD34+/CD38-,15.5% v 5.7%; P=0.008) with a non-significant increase in progenitor cells (HPC; Lin-/CD34+/CD38+, 15.4% v 9.2%; P=0.3). Additionally, PD1+/CD71+ erythroid progenitors (6.5% v 28.1%; P <0.0001)) and granulocytic myeloid derived suppressor cells (MDSC-G (Lin-/CD33+/ CD38-/CD11b+/CD14-); 10 v 23.7%; P=0.001) were significantly decreased in TP53 MT versus WT patients. The percentage of PDL1+ HSC or HPC were similar in HMA-naïve versus HMA-failure or patients actively on HMA (P=0.61 and P=0.84, respectively). More importantly, TP53 MT patients were enriched for an immune suppressive/anergic profile with increased % of TIM3+ MDSC-G (4% v 2%, P=0.04) and decreased % of OX40 cytotoxic T-cells (2.2 v 2.9%; P=0.006). As TP53 MT strongly predicts for inferior OS (P <0.0001), survival was similarly predictive with checkpoint alterations associated with TP53 MT.
Although there was no difference in % of T-regulatory cells (T-regs; CD3+/CD4+/ CD25+/CD127dim/-) in TP53 MT versus WT patients (P=0.75), there was a trend for increased ICOS+ T-regs in TP53 MT patients (16.9% v 13%; P=0.09). Increased ICOS+ T-regs was associated with inferior OS in the total cohort (5.7 v 13.3 months, P=0.003)) and TP53 WT cohort (5.5 months vs NR, P=0.01)). In multivariable analysis incorporating age, BMT status, HMA failure, and revised international prognostic scoring system (IPSS-R) category, increased ICOS+ T-regs remained an independent co-variate for inferior OS in both the total cohort (HR 2.28, 95% CI 1.13 to 4.62; P= 0.02) and TP53 WT cohort (HR 4.69, 95% CI 1.33 to 16.56; P= 0.02)).
Conclusion In patients with MDS and sAML, immune checkpoint expression is heterogeneous in HSCs and immune cell subsets. TP53 mutation portends an immunologically distinct, immune evasive phenotype that may be the predominant driver of their poor prognosis. Increased % of tumor infiltrating ICOS+ T-regs is highly predictive of outcome, independent of TP53 mutation status. We conclude that comprehensive immune checkpoint profiling may offer rationale for targeted immunomodulatory therapeutic strategies.
Sallman: Celgene: Research Funding. Komrokji: Celgene: Honoraria; Novartis: Honoraria, Speakers Bureau. Lancet: Boehringer Ingelheim: Consultancy; Celgene: Consultancy; Bio-Path Holdings: Consultancy; Janssen: Consultancy; Pfizer: Other: Institutional research funding, Research Funding; Erytech: Consultancy; Jazz Pharmaceuticals: Consultancy; BioSight: Consultancy; Novartis: Consultancy. Padron: Incyte: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal